The TuriTap, a new low-tech water chlorination device that operates without electricity, entered a crucial phase of testing in January: a randomized controlled trial across 40 health care facilities in western Kenya.
For Open Philanthropy, this represents a milestone in a journey that began in 2020, when program officers Chris Somerville and Heather Youngs recommended a small grant to our partners at Good Ventures to help UC Berkeley professor Amy Pickering, the TuriTap’s primary inventor, better understand local market needs and opportunities. With the device set for commercial release in Kenya this spring, we wanted to highlight its practical applications and tell the story of how Somerville and Youngs came to support the device. If the TuriTap is adopted more widely throughout sub-Saharan Africa, it could prove to be a valuable tool in reducing the burden of waterborne diseases that currently affect hundreds of millions across the continent.
*****
Hundreds of millions of people worldwide still lack access to clean drinking water. The consequences are severe — the World Health Organization estimates that diarrheal disease kills around 450,000 children each year, with contaminated drinking water being one of the leading causes, alongside contaminated food and poor sanitation. While treatment systems, distribution networks, and wastewater management are key elements to ensure clean water and reduce mortality rates, building this infrastructure is often slow, difficult, and expensive.
Planning a water improvement project means answering myriad questions: does the community have steady access to electricity? Are there preexisting boreholes or pipes? Are the pipes pressurized? Leaky? Are they a year old, or a hundred years old? How many hours a day is water available? Even after infrastructure is built, properly maintaining it remains an ongoing and costly challenge, whether in the U.S. or in low-income countries.
UC Berkeley professor Amy Pickering has spent more than a decade researching how to mitigate the harms of contamination when water supply is intermittent and electricity access is unreliable. After the 2004 Indian Ocean earthquake and tsunami, Pickering assisted relief efforts by installing water treatment systems and solar panels across Sri Lanka. This experience led her to an interdisciplinary PhD program at Stanford, where she focused on human-centered design approaches to water and sanitation infrastructure. Toward the end of her PhD, Pickering started studying how to improve drinking water quality in low-income, densely populated communities in Dhaka, Bangladesh. Although local households received piped water from a central treatment plant, the presence of leaky pipes, inconsistent supply, and low water pressure created a vacuum effect, which sucked in contaminants like sewage through small cracks in the piping.
Pickering explains that recontamination is a common problem with centralized treatment systems: “There’s an expectation that if people are getting water from an improved source, it’s going to be safe,” she says. “But that’s not the case when it’s traveling through intermittent supply systems.”
The problem with point-of-use treatment
Point-of-use treatment — an in-home ceramic filter, or chlorine tablets to treat a household water supply — can help mitigate the problems of patchy infrastructure. But these methods, too, have shortcomings. Yoshika Crider, a postdoctoral fellow on Pickering’s team, explains that the operation and maintenance of household treatments falls on users. Research shows that when treatment requires a change in the user’s behavior, correct use declines over time. Unfortunately, “most of the time” isn’t enough to fully avert the harms of contaminated drinking water. “If you want the health benefits, you need to do those household-level treatment approaches almost 100% of the time,” Crider explains.
This is a common finding in the larger body of research on health behavior: if the uptake needs to be virtually 100%, it’s a likely recipe for failure. Most of us wouldn’t have teeth if the benefits of flossing were all-or-nothing. “It only takes forgetting sometimes to be at risk for waterborne illness,” Crider says. While point-of-use devices can partly compensate for weak infrastructure, hidden costs and declining usage rates within individual households mean they’re far from ideal. In one study, Pickering and co-authors found that the usage rate of an in-home device dropped by 50% once the researchers stopped visiting homes to promote it, even if equipment continued to be delivered for free.
Pickering’s work in Bangladesh led her to think that a better alternative would be a point-of-collection approach: something that would allow people to collect their drinking water as they usually do — from the community tap or borewell, say — without hidden costs or behavioral changes. The more research her team conducted, the more their ideal device started to take shape. To be useful in rural settings, the device couldn’t require electricity. It would need to use liquid chlorine to decontaminate the water, which many communities already have access to in the form of simple dilute bleach.[1]Liquid chlorine can also be made on-site with water, salt, and a little bit of electricity. That’s another reason it’s preferable to chlorine tablets — especially for remote communities without access to global supply chains. And it would need to dispense chlorine automatically (known as “passive chlorination”), so that no behavioral change was required.

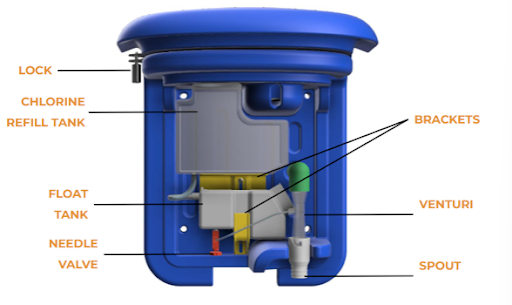
Pickering and her team started designing a device in 2013, cautiously optimistic that they could check all the boxes. In trying to figure out how to get around the need for electricity, Pickering identified a common property of fluid dynamics called the Venturi effect: when water flows through the constrained section of a pipe, the water speeds up and its pressure drops.
This simple physical principle drives Pickering’s device, named the TuriTap. Water passes through a constriction, which causes a small amount of liquid chlorine solution to be suctioned in from a perpendicular tube attached to the constriction. Automated dosing, which is proportional to the flow of water and adjusted with a precise valve, ensures that the proper amount of chlorine is mixed — overuse of chlorine can impact the taste, which is a common problem in large-batch chlorination, and underuse will not disinfect the water sufficiently. The device is also cheap to manufacture, costing only $100 per unit to produce at scale. And crucially, it doesn’t require overhauling existing systems to work.
“Amy’s invention is great in that it works with the existing water distribution system. It doesn’t require huge infrastructure investment,” says Open Philanthropy Program Officer Heather Youngs, who decided with her colleague Chris Somerville to support Pickering’s work with an initial grant in 2020.
Over the last few years, Pickering and her team have continued to hone the device and drive down production costs from the working prototype they had by 2019. They’ve developed a growing evidence base confirming the reliability of point-of-collection devices. In a 2019 randomized controlled trial of 920 households in a low-income, urban environment in Dhaka, Pickering and her team found that passive chlorination of drinking water at the point of collection was associated with a 23% reduction in child diarrhea prevalence. This finding was self-reported, which was a key limitation of the study.
Around the same time, Pickering and her team turned their attention to sub-Saharan Africa. Many households get their water from a dedicated community source, and chlorination is a well-known water treatment method after decades of NGOs marketing household chlorine products. But however effective the TuriTap was in theory, it wouldn’t accomplish much without a viable strategy to manufacture and market the device. This is a common problem: academic grants are usually geared toward research and development rather than market scoping. “It’s difficult to find funds that are directed toward such activities,” Youngs explains. Small business innovation grants are available via the National Institutes of Health, but aren’t usually directed at market assessments or sales modeling. “Not very many funders want to support that type of planning grant,” says Pickering. Funders often assume that the logistics can be figured out without additional resources.
This made Pickering’s initial request for funding to support market scoping somewhat unusual, but her end goal — lessening the burden of diarrheal disease in low-resource settings — seemed like a potentially impactful opportunity. Somerville and Youngs were also excited to lend support to the project because they knew it might struggle to procure funding from elsewhere. “When promising projects fall between the jurisdictions of large funding bodies, we’re sometimes willing to step in,” Somerville says.
With Open Philanthropy’s planning grant, Pickering continued to push forward. Early responses to the TuriTap were promising. Over a six-month trial period during which kiosk owners in Kenya used the TuriTap, the device performed well compared to other in-line chlorinators. Likewise, a 2021 internal report by the NGO Evidence Action, also an Open Phil grantee, produced promising results. The team found the TuriTap dosed more accurately and could be installed on a broader range of infrastructure than the other shortlisted devices.
While the TuriTap won’t be the right choice in every situation, Somerville and Youngs think that the device’s unique combination of using liquid chlorine solution and operating without electricity could fill an important gap in the market.
Randomized controlled trial in Kenyan health care facilities
When Pickering co-authored a 2022 critical review of passive in-line chlorination, she found that other researchers were arriving at the same broad conclusion: passive chlorination works. Based on this growing body of evidence — and the promise of Pickering’s device — Youngs and Somerville continued funding her work. One portion of this second grant is helping to fund an ongoing randomized controlled trial (RCT) to assess the TuriTap’s efficacy in 40 health care facilities across western Kenya; the project is a collaboration between Pickering’s team, CARE, and the Kenya Medical Research Institute. “Health care facilities are sort of an obvious place for an intervention that provides safe water passively,” Crider says. They’re hotspots for antimicrobial-resistant germs, which means basic sanitation is even more important than usual. Hospitals in Kenya are also, in a way, a microcosm for the larger challenges of scaling up water infrastructure. Some have their own boreholes on-site, while others receive municipal water, use a rainwater harvesting system, or use a mix of all three. Each facility is unique.

The team started training and piloting data collection at the end of October 2024, and the study launched in late January 2025. The plan is to collect samples from newborn children and mothers, monitor for pathogens associated with sepsis, and then administer phone surveys to evaluate whether the intervention can reduce the likelihood of participants becoming colonized with harmful pathogens or reporting symptoms of serious infections. Pickering is optimistic about the research: “We think there is huge potential for reducing neonatal mortality and maternal infections, and also reducing the spread of antibiotic-resistant bacteria more broadly in health care facilities,” she says.
In addition to the RCT, the grant will help Pickering and her team optimize for lower in-country manufacturing costs, scale up assembly, and distribute the device in partnership with Davis & Shirtliff, a leading supplier of water equipment in Africa. They’re also seeking certification from Kenya’s Bureau of Standards. If all goes to plan, the TuriTap will be available for purchase in Kenya in late spring. Pickering has also recently co-founded the nonprofit Mangrove Water, which is aimed at providing technical assistance and capacity-building for governments, utilities, and other organizations implementing passive chlorination globally.
Decades from now, Pickering’s vision is for everyone to have 24/7 safe water on tap in their home, delivered by a professional service provider. Pickering hopes that this day will arrive sooner rather than later, but it is far from guaranteed. “The challenges of intermittent supply, especially, will be difficult to overcome in the near future,” she says. In the meantime, passive chlorination devices like the TuriTap could save thousands of lives.
Footnotes
| 1 | Liquid chlorine can also be made on-site with water, salt, and a little bit of electricity. That’s another reason it’s preferable to chlorine tablets — especially for remote communities without access to global supply chains. |
|---|
